Sekce:
Daily overview
VZP on Non-Traded Medical Devices without EMDN
VZP informs applicants about the option to keep non-traded medical devices without EMDN in the Reimbursement Catalogue.
VZP
10/02/2025
Sekce:
Focused on
Dawn of the Amendment to the Act on Public Health Insurance – Part 2
As part of our new article series, we briefly outline the key changes in the medicines domain linked to the amendment to the Act on Public Health Insurance. This instalment focuses on reimbursement...
Pharmeca a.s.
10/01/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 22
Snippets from Analyses Incorporating Deductible Co-payments
Pharmeca a.s.
09/26/2025
Sekce:
Focused on
Dawn of the Amendment to the Act on Public Health Insurance – Part 1
As part of a new article series, we will briefly highlight the main areas that will change under the amendment to the Act on Public Health Insurance, effective 1 January 2026.
Pharmeca a.s.
09/17/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 21
Division of Medicines into Two Separate Reference Indications.
Pharmeca a.s.
09/03/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 20
Replacement of the “S” Symbol Expected to Increase Budget Impact
Pharmeca a.s.
08/20/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 19
Limitation of Reimbursement Amount for Highly Innovative Medicinal Products
Pharmeca a.s.
08/06/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 18
Condition for Previously Reimbursed Indications of Orphan Medicinal Products
Pharmeca a.s.
07/23/2025
Sekce:
Daily overview
VZP Requests Submission of EMDN Codes
VZP requests that all applicants submit EMDN codes for all medical devices (ZÚM) listed in the VZP Reimbursement Catalogue.
VZP
07/16/2025
Sekce:
Data visualization
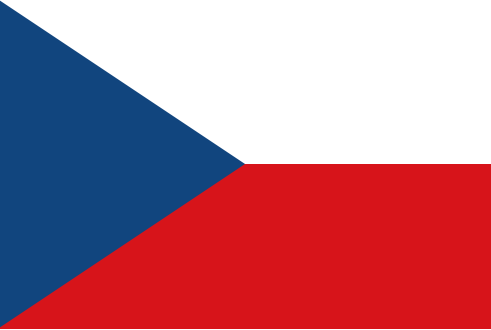
Interactive Map of Countries Used in External Price Referencing of Medicinal Products
An interactive map that visualizes the countries involved in the EPR system as applied in the Czech Republic.


Pharmeca a.s.
07/10/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 17
Reimbursement of a Rare Disease Drug in Combination Therapy
Pharmeca a.s.
07/09/2025
Sekce:
Daily overview
Position of the Ministry of Health of the Czech Republic - indications of Diseases Meeting the Definition of a Rare Disease
Position of the Ministry of Health of the Czech Republic on Administrative Proceedings for Reimbursement Applications for Indications of Diseases Meeting the Definition of a Rare Disease, Involving...
MoH CZ
06/30/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 16
Questions Surrounding Reimbursement for Off-Label Indications
Pharmeca a.s.
06/25/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 15
The Importance of Therapeutic Interchangeability for Ensuring Full Reimbursement Within an Annex No. 2 Group Under the Act on Public Health Insurance
Pharmeca a.s.
06/18/2025
Sekce:
Daily overview
Selection from Decision-Making Practice - 14
Confidential Agreements May Not Be Considered in the Administrative Procedure
Pharmeca a.s.
06/13/2025
Sekce:
Daily overview
Summary Report – Orphan Medicines
The Advisory Board for the Reimbursement of Medicinal Products Intended for the Treatment of Rare Diseases at the Ministry of Health of the Czech Republic has published a summary report evaluating...
MZ ČR
06/06/2025